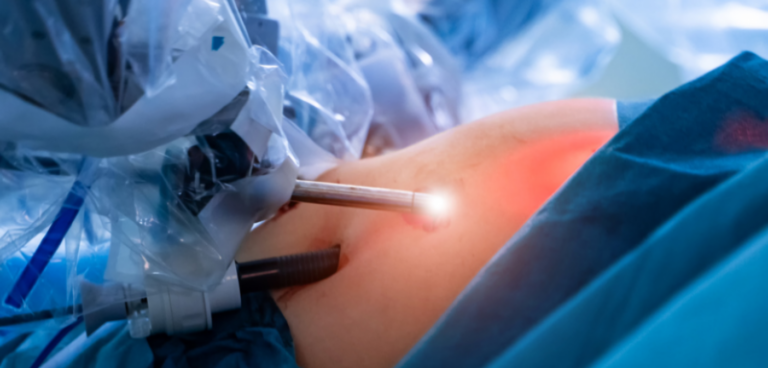
Robot-assisted surgery used to perform bladder cancer removal enables patients to recover more quickly and spend 20% less time in hospital, a first-of-its kind clinical trial led by scientists at University College London (UCL) and the University of Sheffield has concluded.
The study, published in JAMA and funded by The Urology Foundation with a grant from the Champniss Foundation, also found robotic surgery reduced the chance of readmission by half (52%), and revealed a “striking” four-fold (77%) reduction in prevalence of blood clots (deep vein thrombus & pulmonary emboli) – a cause of health decline and morbidity – when compared to patients who had open surgery.
Patients’ physical activity – assessed by daily steps tracked on a wearable smart sensor – stamina and quality of life also increased, the team found.
Researchers said the findings provide the strongest evidence so far of the patient benefit of robot-assisted surgery and are now urging National Institute of Clinical Excellence (NICE) to make it available as a clinical option across the UK for all major abdominal surgeries including colorectal, gastro-intestinal, and gynaecological.
Co-chief investigator, John Kelly, professor of Uro-Oncology at UCL’s division of surgery & interventional science and consultant surgeon at University College London Hospitals, said: “Despite robot-assisted surgery becoming more widely available, there has been no significant clinical evaluation of its overall benefit to patients’ recovery.
“In this study we wanted to establish if robot-assisted surgery, when compared to open surgery, reduced time spent in hospital, reduced readmissions, and led to better levels of fitness and quality of life; on all counts this was shown.
“An unexpected finding was the striking reduction in blood clots in patients receiving robotic surgery; this indicates a safe surgery with patients benefiting from far fewer complications, early mobilisation and a quicker return to normal life.”
Open surgery remains the NICE “gold standard” recommendation for highly complex surgeries, though the research team hope this could change.
Kelly added: “In light of the positive findings, the perception of open surgery as the gold standard for major surgeries is now being challenged for the first time.
“We hope that all eligible patients needing major abdominal operations can now be offered the option of having robotic surgery.”
Across nine UK hospitals, 338 patients with non-metastatic bladder cancer were randomised into two groups: 169 patients had robot-assisted radical cystectomy (bladder removal) with intracorporeal reconstruction (process of taking section of bowel to make new bladder), and 169 patients had open radical cystectomy.
The trial’s primary endpoint was length of stay in hospital post-surgery. On average, the robot-assisted group stayed eight days in hospital, compared to 10 days for the open surgery group – so a 20% reduction. Readmittance to hospital within 90 days of surgery was also reduced – 21% for the robot-assisted group vs 32% for open.
A further 20 secondary outcomes were assessed at 90 days, six- and 12-months post-surgery. These included blood clot prevalence, wound complications, quality of life, disability, stamina, activity levels, and survival (morbidity). All secondary outcomes were improved by robot-assisted surgery or, if not improved, almost equal to open surgery.
This study, and previous studies, showed both robot-assisted and open surgery are equally as effective in regards cancer recurrence and length of survival.
The research team is now conducting a health economic analysis to establish the quality-adjusted life year, which incorporates the impact on both the quantity and quality of life.