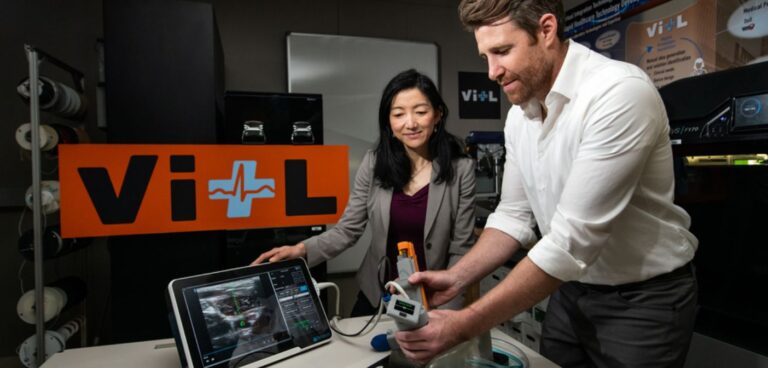
Engineers at the Massachusetts Institute of Technology (MIT) have developed an AI-powered device that could help first responders deliver complex medical interventions at the point of injury.
Together with physicians from the Center for Ultrasound Research and Translation (CURT) at Massachusetts General Hospital, researchers developed a solution which could be deployed in the small window of time medical professionals have to apply lifesaving treatment to victims with severe internal bleeding.
The Artificial Intelligence–Guided Ultrasound Intervention Device (AI-GUIDE) is a handheld platform that has the potential to help personnel with simple training to quickly install a catheter into a common femoral vessel, enabling rapid treatment.
“Simplistically, it’s like a highly intelligent stud-finder married to a precision nail gun,” said Matt Johnson, a research team member from the laboratory’s Human Health and Performance Systems Group.
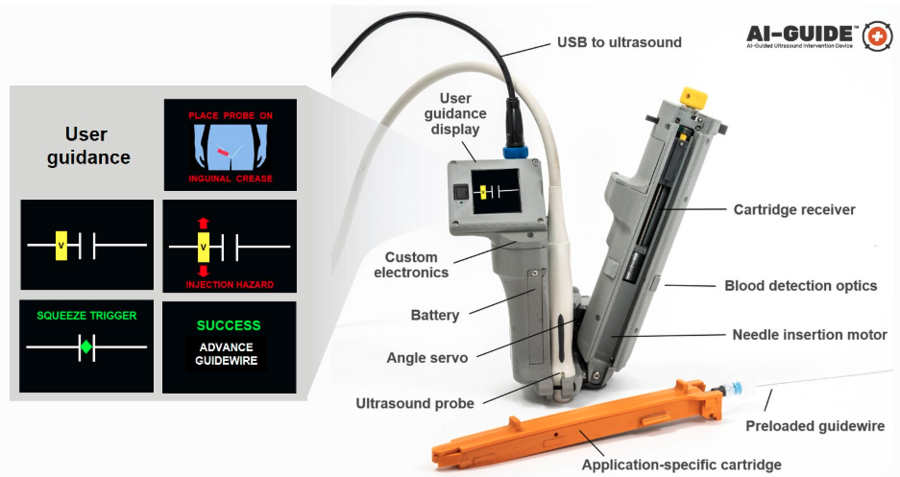
AI-GUIDE is made of custom-built algorithms and integrated robotics that could pair with most commercial portable ultrasound devices.
The Lincoln Laboratory team developed the AI in the device by leveraging technology used for real-time object detection in images.
“Using transfer learning, we trained the algorithms on a large dataset of ultrasound scans acquired by our clinical collaborators at MGH,” explained Lars Gjesteby, a member of the laboratory’s research team. “The images contain key landmarks of the vascular anatomy, including the common femoral artery and vein.”
These algorithms interpret the visual data coming in from the ultrasound that is paired with AI-GUIDE and then indicate the correct blood vessel location to the user on the display.
“The beauty of the on-device display is that the user never needs to interpret, or even see, the ultrasound imagery,” added Mohit Joshi, the team member who designed the display. “They are simply directed to move the device until a rectangle, representing the target vessel, is in the centre of the screen.”
To ensure that the needle reliably punctures the vessel, the team engineered the device to be able to check its own work.
“When AI-GUIDE injects the needle toward the centre of the vessel, it searches for the presence of blood by creating suction,” said Josh Werblin, the program’s mechanical engineer. “Optics in the device’s handle trigger when blood is present, indicating that the insertion was successful.” This technique is part of why AI-GUIDE has shown very high injection success rates, even in hypotensive scenarios where veins are likely to tent.
Recently, the team published a paper in the journal Biosensors that reports on AI-GUIDE’s needle insertion success rates. Users with medical experience ranging from zero to greater than 15 years tested AI-GUIDE on an artificial model of human tissue and blood vessels and one expert user tested it on a series of live, sedated pigs. The team reported that after only two minutes of verbal training, all users of the device on the artificial human tissue were successful in placing a needle, with all but one completing the task in less than one minute.
The team is continuing to test the device and work on fully automating every step of its operation. In particular, they want to automate the guidewire and catheter insertion steps to further reduce risk of user error or potential for infection.