Advancements in medical technology are creating a world where robots may play a bigger part in healing the sick than doctors.
According to a 2019 research report by MarketsandMarkets, the global medical robot market is projected to reach £13.2bn by 2023 from an estimated £5.1m in 2018. Key factors propelling the growth of the market include technological advancements in medical robots, advantages offered by robot-assisted training in rehabilitation therapy, increase in funding for medical robot research, and the issuance of IPOs by medical robot companies. What’s more, rapid growth in the geriatric population and rising patient preference for minimally invasive surgeries could offer further growth during the forecast period.
In the UK, a new surgical robotic system has been used to successfully perform minimal access surgery (MAS) – also referred to as keyhole or laparoscopic surgery – on patients at two NHS hospitals. According to its maker, the solution could result in wider use of robotic MAS than seen to date – currently across Europe only 13% of hysterectomy procedures are reportedly conducted laparoscopically.
Developed by Cambridge-headquartered CMR Surgical, the solution, called Versius, has so far performed a range of colorectal surgeries, helping to treat patients with bowel disease or bowel cancer. Specifically, three independent arms, which replicate those of a human in size and shape, are coupled with 3D visualisation and unique instrument controls that allow the surgeon to mimic their own human movement, enabling precise surgeries and less strenuous procedures.
MAS is associated with a number of potential benefits compared to open surgery, including the ability to reduce rates of surgical site infections, pain and scarring. It is also linked to faster recovery in hospital, with fewer post-operative bed days required for recovery. For example, a 2018 report by the Office of Health Economics found that a shift to MAS led to a reduction in the average length of stays for gynaecology patients from 5.5 days to 1.5 days in 95% of cases.
Western General Hospital in Edinburgh and Milton Keynes University Hospital NHS Trust in Buckinghamshire are the first medical facilities to use Versius in Europe; however, further NHS hospitals are scheduled to introduce the system in 2020. These include both large teaching hospitals and smaller local centres.
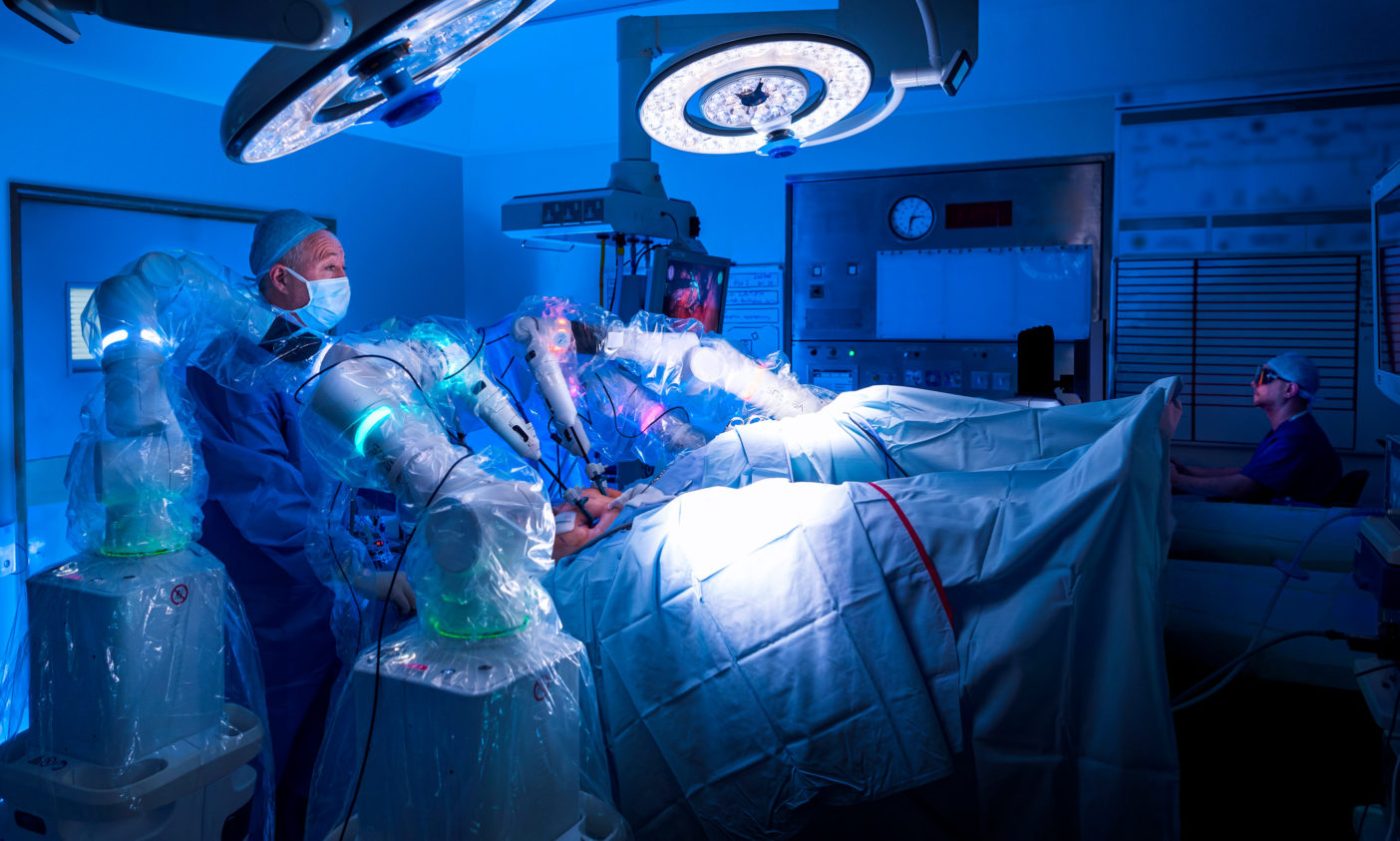
According to Mark Slack, chief medical officer at CMR Surgical, part of Versius’ appeal is that the system has been designed to be portable, allowing it to be moved to different sites within a hospital, or transported between hospitals within an NHS trust. Furthermore, once in theatre, it takes, on average, 15 minutes to set up the system.
“We set out to design a system that was versatile, portable and cost-effective, and it is immensely rewarding to see it now being used in the NHS – one of the most thorough and clinically rigorous health systems in the world,” says Slack.
“We are intent on ensuring the responsible introduction of this technology, and the skilled expertise and focus on innovative research at these NHS sites make them the ideal place for this technology. Our focus now will be on working with the surgical community across the UK to provide the option of minimal access surgery to everyone who may benefit.”
Across its first two NHS sites, Versius – which can be purchased at a fixed cost through a Managed Service Agreement – has the potential to perform up to 700 MAS procedures each year, which otherwise may have been performed by open surgery.
Dr Tracey Gillies, medical director, NHS Lothian, which governs Western General Hospital, says the facility is delighted to be to the be the first in Europe to pioneer this new type of robotic surgery. “This is a really exciting development and is a credit to the team, who are determined to push boundaries to provide the best patient care possible.”
Likewise, Professor Joe Harrison, chief executive at Milton Keynes University Hospital NHS Foundation Trust, believes such robotic systems are set to play a vital role in delivering world-leading surgical care across the NHS. “The hope for us is that this will lead to better outcomes for patients as well as helping us to free up bed space that can then be used to help others in need.”
As part of the introduction of Versius, a clinical registry has been established to provide a database of patient outcomes information to support patient safety, as well as technical data that can support assisted learning and help optimise the system’s use in the future.
Beyond surgery
But it’s not just within operating theatres where robots are positively impacting the NHS. North Bristol NHS Trust (NBT) and Bristol Robotics Laboratory at the University of the West of England (UWE) are collaborating on the development of robotics and other healthcare technology to improve patients’ health and hospital experience.
Under the NBT/UWE Health Technology partnership, announced in January 2020, NBT is considering how emerging technologies, such as AI, machine learning, and socially and physically assistive robots, could be used to better support patients at Southmead Hospital in Bristol. It is also trialling technology with patients and care staff, leveraging benefits of shared facilities, and supporting and facilitating joint research and learning.
According to NBT, Southmead Hospital is one of the most technologically advanced in Europe, with robots conducting cancer surgery, dispensing pharmacy medicines, transporting supplies, and analysing blood samples. However, the introduction of socially assistive robots could give post-operative patients on Southmead’s wards personalised guidance to regularly eat, drink and exercise, helping them to recover physically and mentally in conjunction with their therapy team.

North Bristol NHS Trust clinical director for anaesthesia, surgery, critical care and renal, Tim Whittlestone, says: “We have an ageing population requiring ever more complex treatment. Technology gives our growing workforce massive opportunities to manage this and improve care.
“Robots can help us do some of the more mundane, repeatable tasks and free up staff to do what they do best – listening, thinking and caring. They can also analyse data, helping us to really personalise treatment, care and recovery. There are constant developments, so we need work out how patients and staff interact with the technology and whether it’s useful.”
Currently, 12 automated guided vehicles transport food, linen, medicines and other supplies around the hospital 24/7. Steered by GPS and operating lifts, they have reportedly quickened deliveries to wards and reduced injuries to porters. Elsewhere, the hospital’s pathology lab uses automated technology to move and test blood samples, after they are transported underground via pneumatic tube from wards. Southmead’s pharmacy also uses three automated robots to sort and select medicines for dispensing by pharmacists.
Clinicians are also exploring the introduction of an algorithm to predict seasonal variations in admissions to Southmead’s emergency department, as well as AI-assisted reading of breast mammograms and decision-making on prostate cancer. What’s more, the Bristol Robotics Laboratory team is seeking joint funding to further develop assistive robotic systems such as CHIRON, which is being designed to support older adults with mobility and other ageing-related impairments.
Southmead Hospital staff will help shape the design and safety testing of the CHIRON technology, thus accelerating its development and ensuring it fits in with clinical procedures and practices. It’s thought that the robot could eventually assist with anything from bringing a tray of food or drink to a patient on demand, to helping those with mobility issues to their feet and practise walking to aid their recovery.
Professor Praminda Caleb-Solly, leading research in assistive robotics and intelligent health technologies at Bristol Robotics Laboratory, said: “Hospitals are likely to be the first adopters of this type of technology so it will be beneficial to test our prototype in a hospital setting and work with hospital staff in shaping it. Through this partnership, we can have a more clinically-informed focus to our research and make it more relevant to the specific needs of the patients and NHS staff.”
Research revolution
Robotic automation is also having a transformative effect on medical science. In the USA, a Rutgers University–developed blood-sampling robot has reportedly performed as well or better than people in a world-first human clinical trial of an automated blood drawing and testing device.The device is said to have exceeded clinical standards, with an overall success rate of 87% for the 31 participants whose blood was drawn. For the 25 people whose veins were easy to access, the success rate was 97%.
The device includes an ultrasound image-guided robot that draws blood from veins. According to Josh Leipheimer, a biomedical engineering doctoral student at Rutgers University who was involved in the trial, a fully integrated device, which includes a module that handles samples and a centrifuge-based blood analyser, could be used at bedsides and in ambulances, emergency rooms, clinics, doctors’ offices and hospitals.
“A device like ours could help clinicians get blood samples quickly, safely and reliably, preventing unnecessary complications and pain in patients from multiple needle insertion attempts,” says Leipheimer, adding that the device could also be used in such procedures as IV catheterisation, central venous access, dialysis and placing arterial lines.
Elsewhere, researchers at the University of Dundee, in Scotland, have developed an automated robotic screening system to rapidly test the effect of drugs and other chemicals on human sperm. Led by Professor Chris Barratt and Dr Paul Andrews, the research team at Dundee is working towards finding a safe and effective male contraceptive.
Featuring a miniaturised parallel testing system run by a robot, the automated system uses a fast microscope and image-processing tools that precisely track the very fast movement of human sperm, thus allowing the effects of drugs to be accurately measured. The system, which speeds up the process of drug hunting several thousand-fold, was used to rapidly test the efficacy of the ReFRAME collection, one of the world’s largest collections of previously approved and clinically tested drugs.
In total, around 13,000 drugs were tested to gauge their impact on both the motility (movement) and acrosome reaction (essential for fertilisation) of human sperm. Dr Andrews, who leads the National Phenotypic Screening Centre in Dundee, says: “The conventional way to test drugs for contraceptive activity is prohibitively time-consuming, but we have managed to develop a disruptive technology platform we hope will be a game changer.”
This article originally appeared in the April 2020 issue of Robotics & Innovation magazine